The patient had a history of multiple myeloma, prostate cancer, & CHF.
Discussion
This case highlights not only T2Bacteria’s benefit of rapid identification but also the ability to detect the causative organism in the presence of antibiotics as this patient had received the dose of vancomycin before the T2Bacteria was drawn.
Utilization of the T2Bacteria test allows for directed therapy on the same day as the identification of suspected infection. In this case, it took almost 48 hours from admission to identify S. aureus in the blood (Day 3 of admission). Ordering T2Bacteria at 24 hours after admission allowed appropriate therapy to be started on Day 2. Had T2Bacteria had been ordered simultaneously with blood culture, appropriate therapy could have been started on Day 1.
Initial Presentation
A high-risk patient was admitted with pulmonary edema and suspected pneumonia. The patient had a history of multiple myeloma, prostate cancer, and CHF. Blood cultures were obtained, and the patient was started on intravenous antibiotics for coverage of pneumonia.
Evaluation and Treatment Decision
Empiric Therapy
The patient was started on levofloxacin and piperacillin/tazobactam for empiric coverage of pneumonia.
Blood Culture Result
Twenty-four hours after admission, the nursing unit was called with a critical result from microbiology: gram-positive cocci in clusters.
Updated Therapy
The physician was notified, and a single dose of vancomycin was ordered.
T2Bacteria Result
The physician was uncertain if the organism might be a contaminating organism such as Staphylococcus epidermidis or a more concerning pathogen such as Staphylococcus aureus. The nurse suggested ordering T2Bacteria, and four hours later, the T2Bacteria resulted as S. aureus prompting the appropriate continued therapy with vancomycin. S. aureus was confirmed by the blood culture result the following morning.
Decision Making Based on T2Bacteria Result
The T2Bacteria Panel was used to detect the presence of S. aureus, allowing appropriate therapy to be initiated one day earlier than using blood culture alone.
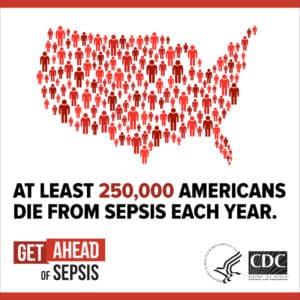
 In the decade and a half since Dr. Nathan wrote these words, the standard of care has remained mired in “19th-century methods.” Despite important diagnostic improvements made to post-blood culture methods, the days-long culturing of blood remains the foundation for pathogen-specific identification. Since clinicians cannot wait days to act when confronted with a patient suspected of sepsis, the standard of care remains empiric therapy. In the 2018 book,
In the decade and a half since Dr. Nathan wrote these words, the standard of care has remained mired in “19th-century methods.” Despite important diagnostic improvements made to post-blood culture methods, the days-long culturing of blood remains the foundation for pathogen-specific identification. Since clinicians cannot wait days to act when confronted with a patient suspected of sepsis, the standard of care remains empiric therapy. In the 2018 book, 